Unveiling the Science: Commonly Researched Typical Dosages for Peptides in 2025
The fascinating world of peptides continues to expand its horizons in scientific research, offering promising avenues for understanding complex biological processes. For any researcher embarking on studies involving these potent compounds, a fundamental understanding of dosages for peptides, including specifics like dosage IPA, dosage TESA, dosage cjc1295, and the practical aspects of how to reconstitute glp3, is not just beneficial—it’s absolutely critical. Improper dosing or reconstitution can skew research results, compromise peptide integrity, and invalidate an entire study. This comprehensive guide, updated for 2025, delves into the typical administration schedules, reconstitution techniques, and common volumes used in research settings for some of the most frequently studied peptides.
Peptides are short chains of amino acids, the building blocks of proteins, that play vital roles as signaling molecules in the body. Their precision and specificity make them invaluable tools in scientific inquiry, allowing researchers to target particular pathways and observe their effects. However, their potency necessitates meticulous handling and accurate measurement to ensure the integrity and reliability of experimental data.
Key Takeaways
- Accurate Reconstitution is Paramount: Proper mixing with bacteriostatic water and gentle handling prevents degradation and ensures accurate dosing.
- Dosages Vary Widely: Peptide dosages are highly specific to the peptide, research goal, and subject, typically ranging from micrograms to milligrams daily or weekly.
- Insulin Syringes are Essential: Precise measurement of reconstituted peptides is achieved using U-100 insulin syringes, understanding the units to volume conversion.
- Storage Impacts Stability: Correct storage conditions for both lyophilized and reconstituted peptides are crucial for maintaining potency and extending shelf life.
- Common Peptides have Established Ranges: Ipamorelin, tesa, and CJC-1295 (with and without DAC) have well-documented research dosage ranges for various applications.
Mastering Peptide Reconstitution: The Foundation of Accurate Dosages
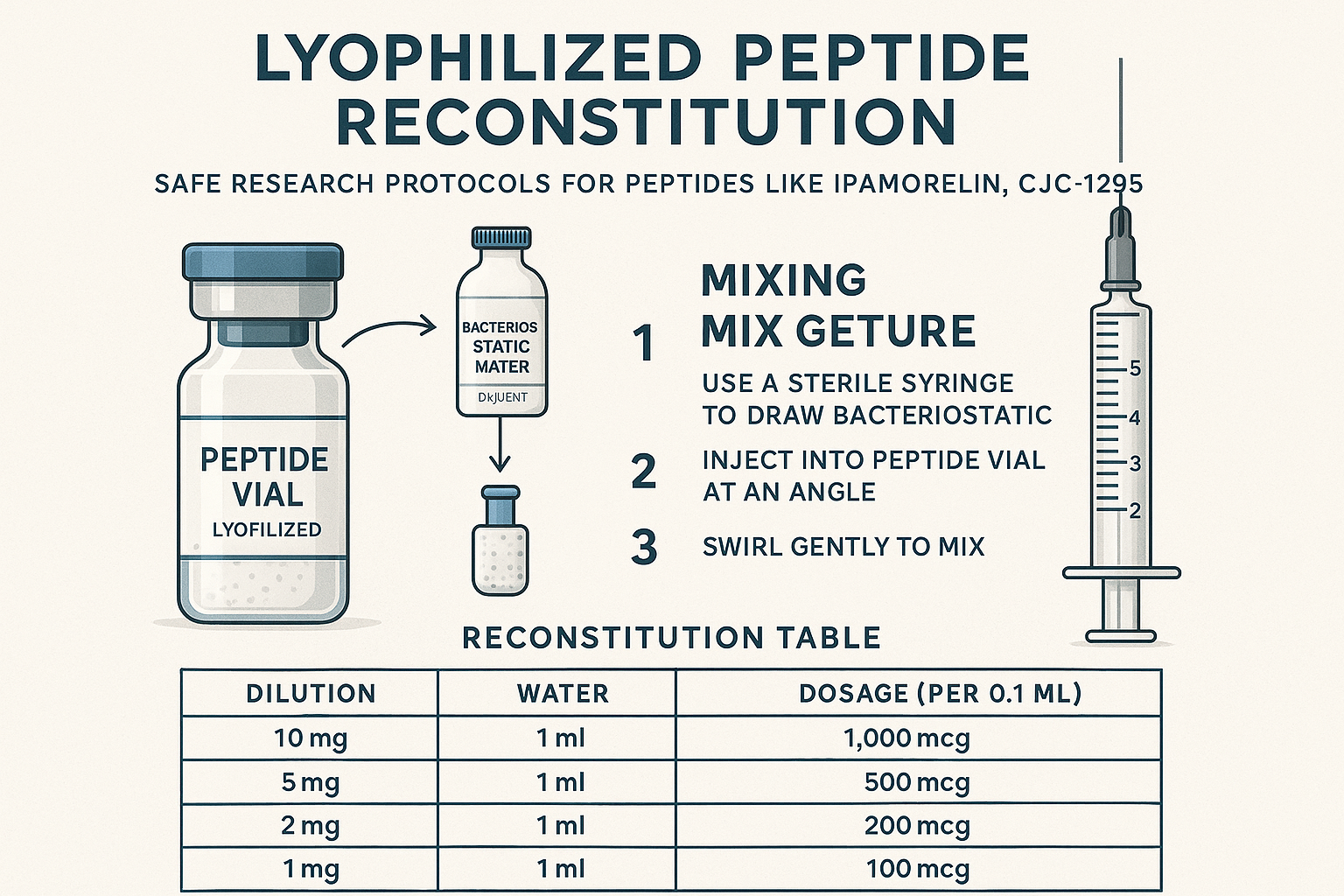
Before any peptide can be administered in a research setting, it must first be reconstituted from its lyophilized (freeze-dried) powder form into a liquid solution. This initial step is foundational to accurate dosages for peptides and demands careful attention to detail.
Understanding Lyophilized Peptides
Most research peptides are supplied as lyophilized powders. This state enhances their stability, allowing for longer storage at appropriate temperatures (typically refrigerated). However, this also means they are not immediately ready for use. The process of reconstitution involves adding a sterile diluent, most commonly bacteriostatic water, to dissolve the peptide powder and create a usable solution.
The Role of Bacteriostatic Water
Bacteriostatic water (BW) is the preferred diluent for peptide reconstitution. It is sterile water containing 0.9% benzyl alcohol, which acts as a bacteriostatic preservative, inhibiting the growth of most common contaminating bacteria. This preservative quality is crucial for multi-dose vials, as it helps maintain sterility for several weeks after reconstitution, provided proper aseptic techniques are followed.
Step-by-Step Reconstitution Process
- Gather Supplies:
- Lyophilized peptide vial
- Bacteriostatic water vial
- Sterile insulin syringes (typically 1ml, U-100)
- Alcohol wipes
- Gloves (for aseptic technique)
- Calculate Diluent Volume: This is a critical step. To achieve a manageable concentration for precise dosing, researchers must determine the amount of bacteriostatic water needed. A common goal is to make 100mcg (micrograms) equivalent to a specific marking on an insulin syringe (e.g., 10 units on a U-100 syringe).Let’s consider a common example: a 5mg (5000mcg) vial of peptide.
If you want 100mcg to be 10 units on a U-100 syringe:- 10 units on a U-100 syringe is 0.1ml (since 100 units = 1ml).
- So, if 0.1ml contains 100mcg, then 1ml would contain 1000mcg (1mg).
- To make a 5mg (5000mcg) vial into a solution where 1ml = 1mg, you would need 5ml of bacteriostatic water.
A simpler way to think about it for typical vials:
- For a 2mg vial: Adding 2ml of BW makes 10 units = 100mcg.
- For a 5mg vial: Adding 5ml of BW makes 10 units = 100mcg.
- For a 10mg vial: Adding 10ml of BW makes 10 units = 100mcg.
This 10 units = 100mcg ratio is very common and convenient for precise micro-dosing.
- Prepare Vials:
- Remove the plastic caps from both the peptide vial and the bacteriostatic water vial.
- Wipe the rubber stoppers of both vials thoroughly with alcohol wipes and allow them to air dry.
- Draw Bacteriostatic Water:
- Using a sterile insulin syringe, draw the calculated amount of bacteriostatic water from its vial. It’s important to draw slightly more than needed and then push the plunger to the exact mark, expelling any air bubbles.
- Inject into Peptide Vial:
- Carefully insert the syringe needle into the rubber stopper of the peptide vial.
- Slowly depress the plunger, allowing the bacteriostatic water to gently trickle down the inside wall of the peptide vial. Do NOT inject directly onto the lyophilized powder with force, as this can degrade the peptide structure.
- Gentle Mixing:
- Once all the bacteriostatic water has been added, do NOT shake the vial vigorously. Instead, gently swirl the vial between your fingers or roll it between your palms. The goal is to allow the peptide to dissolve naturally. This process may take a few minutes.
- Some researchers prefer to let the vial sit in the refrigerator for 15-30 minutes after initial swirling to ensure complete dissolution.
- Storage of Reconstituted Peptide:
- Once reconstituted, the peptide solution should be stored in a refrigerator (typically 2-8°C or 36-46°F).
- Protect the vial from light, ideally by storing it in its original box or a dark container.
- The shelf life of reconstituted peptides can vary, but generally, they are stable for 2-4 weeks when properly stored. Always refer to specific peptide guidelines for optimal storage. Understanding proper storage is as vital as the initial reconstitution; for more details on this, explore best practices for storing research peptides.
Pull Quote: “Accuracy in peptide research begins with meticulous reconstitution. A rushed or improper mixing technique can compromise the integrity of the peptide, rendering subsequent dosages unreliable.”
Typical Dosages for Commonly Researched Peptides
The specific dosages for peptides can vary significantly based on the research objective, the specific peptide being studied, and the experimental model. It’s crucial for researchers to consult existing literature and established protocols. However, here we will outline commonly researched typical dosage ranges for several popular peptides, along with their usual administration frequency and syringe volumes based on the common reconstitution method described above (10 units = 100mcg).
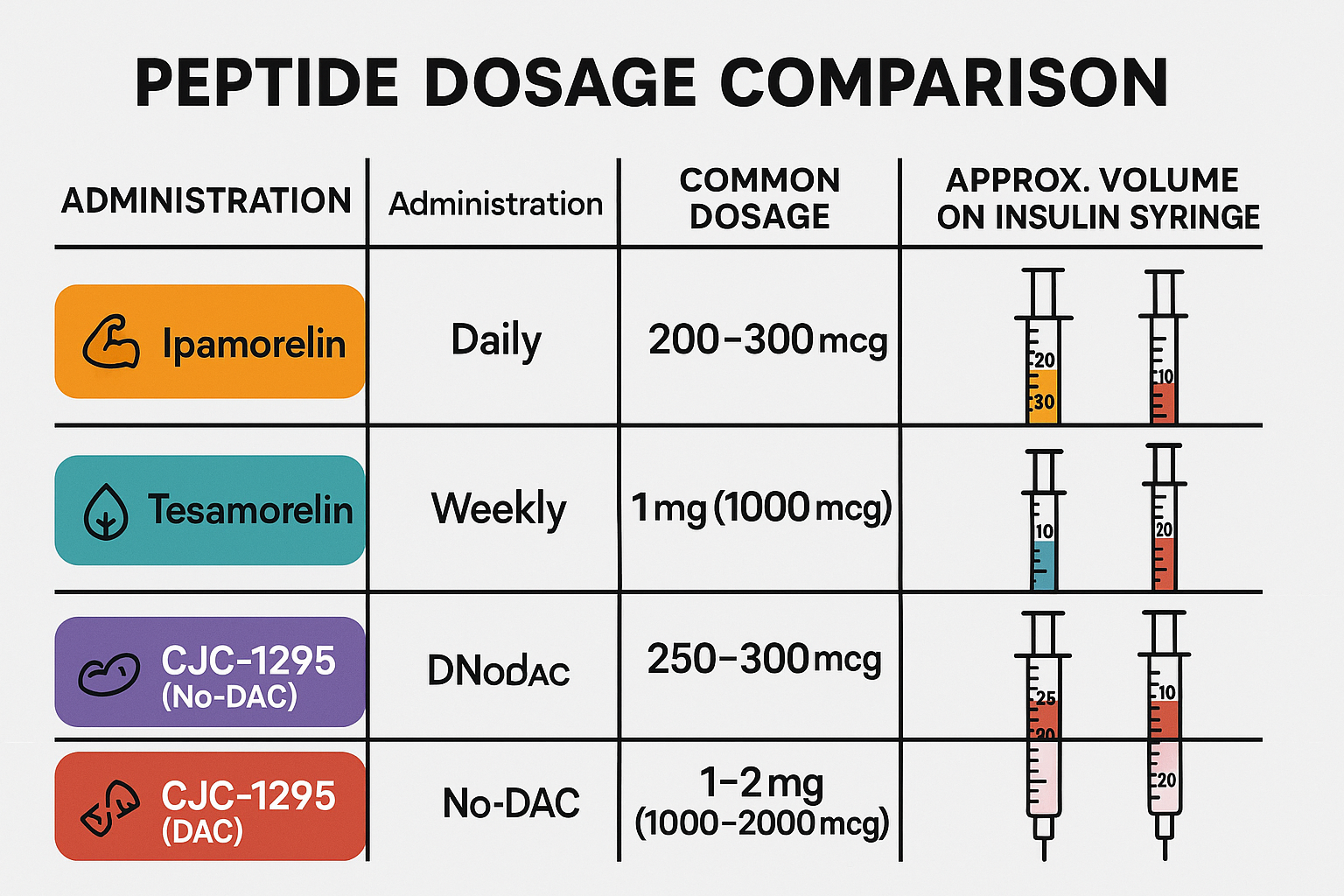
1. Ipamorelin Dosage
Ipamorelin is a growth hormone-releasing peptide (GHRP) that stimulates the pituitary gland to release natural growth hormone. It’s known for its selective action, minimizing the release of cortisol and prolactin, which can be a concern with other GHRPs.
- Research Applications: Often studied for its potential effects on muscle growth, fat reduction, improved sleep quality, and anti-aging properties.
- Typical Dosage Range: 200mcg – 300mcg per day.
- Frequency: Often administered once or twice daily. Some protocols suggest administering it before bedtime due to its potential impact on sleep-related GH pulses.
- Reconstitution Example (2mg vial): If a 2mg (2000mcg) vial is reconstituted with 2ml of bacteriostatic water, the concentration is 1000mcg/ml.
- To administer 200mcg: you would draw 20 units (0.2ml) on a U-100 insulin syringe.
- To administer 300mcg: you would draw 30 units (0.3ml) on a U-100 insulin syringe.
- Syringe Volume (based on 10 units = 100mcg):
- 200mcg = 20 units (0.2ml)
- 300mcg = 30 units (0.3ml)
2. tesa Dosage
tesa is a synthetic peptide that mimics Growth Hormone-Releasing Hormone (GHRH). It is specifically known for its ability to reduce excess abdominal fat (visceral adipose tissue) in individuals with HIV-associated lipodystrophy, but it is also researched for other potential metabolic and cognitive benefits.
- Research Applications: Primarily studied for fat metabolism, particularly visceral fat reduction, and increasingly for its potential neurological effects and cardiovascular benefits.
- Typical Dosage Range: 1mg – 2mg (1000mcg – 2000mcg) per day.
- Frequency: Administered once daily, typically at bedtime.
- Reconstitution Example (5mg vial): If a 5mg (5000mcg) vial is reconstituted with 5ml of bacteriostatic water, the concentration is 1000mcg/ml.
- To administer 1mg (1000mcg): you would draw 100 units (1ml) on a U-100 insulin syringe.
- To administer 2mg (2000mcg): you would need two full U-100 insulin syringes (or 2ml total).
- Syringe Volume (based on 10 units = 100mcg):
- 1000mcg (1mg) = 100 units (1ml)
- 2000mcg (2mg) = 200 units (2ml) – often requiring two injections or a larger syringe.
3. CJC-1295 Dosage (with and without DAC)
CJC-1295 is another synthetic GHRH analog, but it comes in two main forms: with DAC (Drug Affinity Complex) and without DAC (often referred to as Mod GRF 1-29). The presence of DAC significantly prolongs the half-life of the peptide, changing its administration frequency. Exploring the differences between these versions, such as with CJC-1295 DAC muscle research themes, is crucial for researchers.
CJC-1295 with DAC
- Research Applications: Prolonged growth hormone release, often studied for muscle repair, fat loss, and overall anti-aging effects due to its sustained action.
- Typical Dosage Range: 1mg – 2mg (1000mcg – 2000mcg) per week.
- Frequency: Administered once or twice per week due to its extended half-life (around 6-8 days).
- Reconstitution Example (2mg vial): If a 2mg (2000mcg) vial is reconstituted with 2ml of bacteriostatic water, the concentration is 1000mcg/ml.
- To administer 1mg (1000mcg): you would draw 100 units (1ml) on a U-100 insulin syringe.
- To administer 2mg (2000mcg): you would draw 200 units (2ml) on a U-100 insulin syringe.
- Syringe Volume (based on 10 units = 100mcg):
- 1000mcg (1mg) = 100 units (1ml)
- 2000mcg (2mg) = 200 units (2ml)
CJC-1295 without DAC (Mod GRF 1-29)
- Research Applications: Stimulates pulsatile growth hormone release, often paired with a GHRP like Ipamorelin for synergistic effects on muscle growth, fat metabolism, and recovery. The shorter half-life allows for more physiological pulsing. Learn more about the synergy of CJC-1295 and Ipamorelin.
- Typical Dosage Range: 100mcg – 200mcg per day.
- Frequency: Administered once to three times daily, often timed with GHRP administration and typically before meals or bedtime.
- Reconstitution Example (2mg vial): If a 2mg (2000mcg) vial is reconstituted with 2ml of bacteriostatic water, the concentration is 1000mcg/ml.
- To administer 100mcg: you would draw 10 units (0.1ml) on a U-100 insulin syringe.
- To administer 200mcg: you would draw 20 units (0.2ml) on a U-100 insulin syringe.
- Syringe Volume (based on 10 units = 100mcg):
- 100mcg = 10 units (0.1ml)
- 200mcg = 20 units (0.2ml)
Other Commonly Researched Peptides and Their Dosages
While Ipamorelin, tesa, and CJC-1295 are very popular, many other peptides are extensively studied, each with its own dosage considerations.
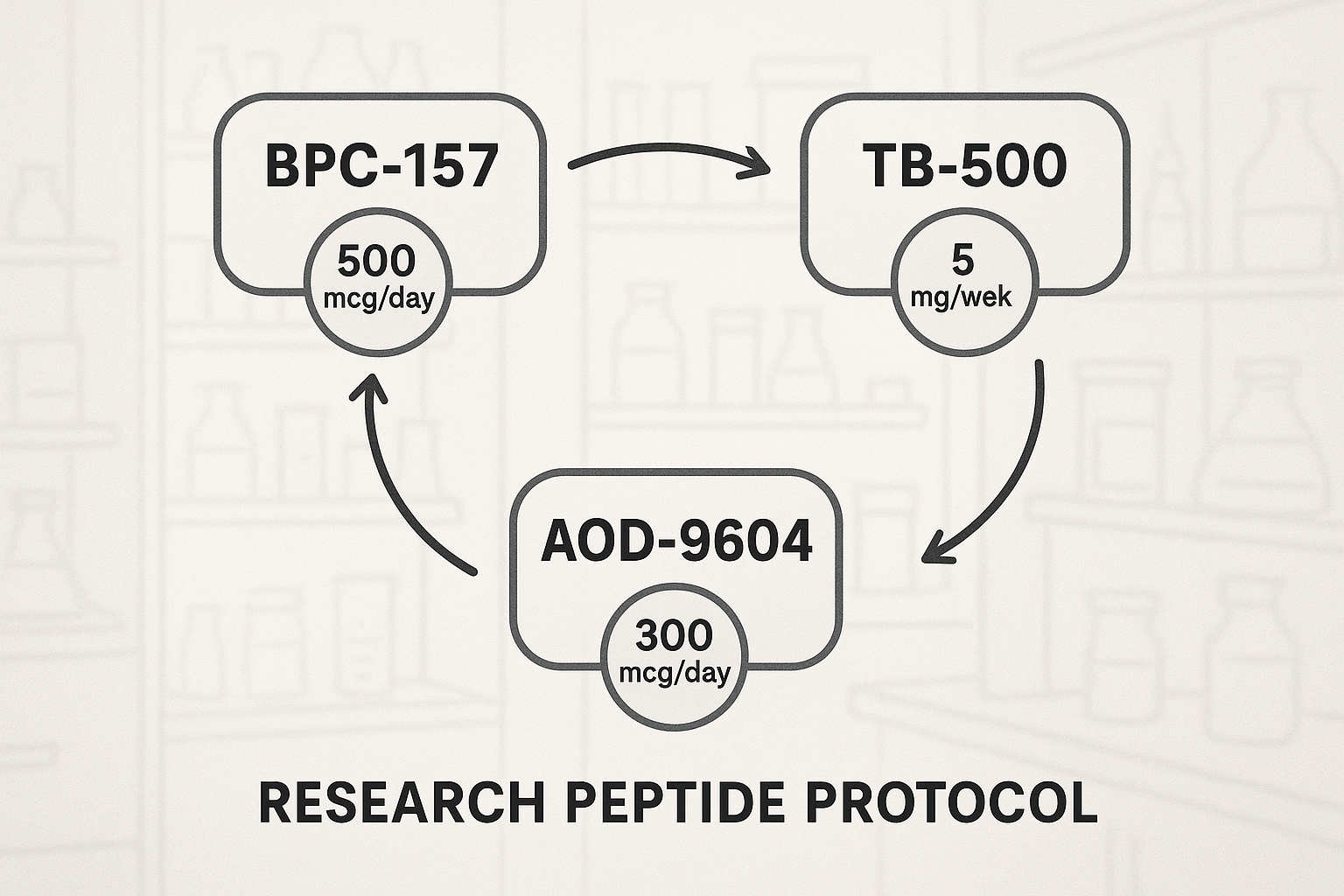
- BPC-157 (Body Protection Compound):
- Research Applications: Wound healing (muscle, tendon, ligament, gut), anti-inflammatory effects, organ protection. Learn more about BPC-157 research themes.
- Typical Dosage Range: 200mcg – 500mcg per day.
- Frequency: Once or twice daily. Some protocols suggest localized administration for specific injury sites.
- Syringe Volume (based on 10 units = 100mcg for a 5mg vial reconstituted with 5ml BW):
- 200mcg = 20 units (0.2ml)
- 500mcg = 50 units (0.5ml)
- TB-500 (Thymosin Beta 4):
- Research Applications: Healing, tissue repair, anti-inflammatory, cell migration, flexibility. Often studied in conjunction with BPC-157.
- Typical Dosage Range: 2mg – 5mg per week.
- Frequency: Often administered as a loading phase (e.g., 2-5mg twice a week for 4-6 weeks) followed by a maintenance phase (e.g., 2-4mg once a month).
- Reconstitution Example (5mg vial): If a 5mg (5000mcg) vial is reconstituted with 5ml of bacteriostatic water, the concentration is 1000mcg/ml.
- Syringe Volume (based on 10 units = 100mcg):
- 2mg (2000mcg) = 200 units (2ml)
- 5mg (5000mcg) = 500 units (5ml) – likely requiring multiple syringes.
- AOD-9604 (Anti-Obesity Drug):
- Research Applications: Fat loss, particularly targeting adipose tissue. It is a modified fragment of the growth hormone molecule.
- Typical Dosage Range: 200mcg – 400mcg per day.
- Frequency: Once daily.
- Syringe Volume (based on 10 units = 100mcg for a 5mg vial reconstituted with 5ml BW):
- 200mcg = 20 units (0.2ml)
- 400mcg = 40 units (0.4ml)
- Epitalon:
- Research Applications: Anti-aging, telomere lengthening, sleep regulation, antioxidant effects.
- Typical Dosage Range: 5mg – 10mg per 10-20 day cycle.
- Frequency: Often administered daily for a short cycle, then periods off.
- Reconstitution Example (10mg vial): If a 10mg (10000mcg) vial is reconstituted with 5ml of bacteriostatic water, the concentration is 2000mcg/ml.
- To administer 5mg (5000mcg): you would draw 250 units (2.5ml) on a U-100 insulin syringe.
- To administer 10mg (10000mcg): you would draw 500 units (5ml) on a U-100 insulin syringe.
- Syringe Volume (based on 10 units = 100mcg; this requires a different BW volume for 10 units=100mcg, so let’s adjust for a practical example):
- If 10mg vial reconstituted with 10ml BW (1000mcg/ml):
- 5mg = 500 units (5ml)
- 10mg = 1000 units (10ml) – clearly indicating the need for careful planning regarding total volume.
- If 10mg vial reconstituted with 10ml BW (1000mcg/ml):
It’s critical to note that these are typical research dosages and should not be interpreted as medical advice or recommendations for human use. All peptide research should be conducted in accordance with ethical guidelines and appropriate regulatory frameworks. For a broader selection of research peptides, you can review the full all peptides for sale catalog.
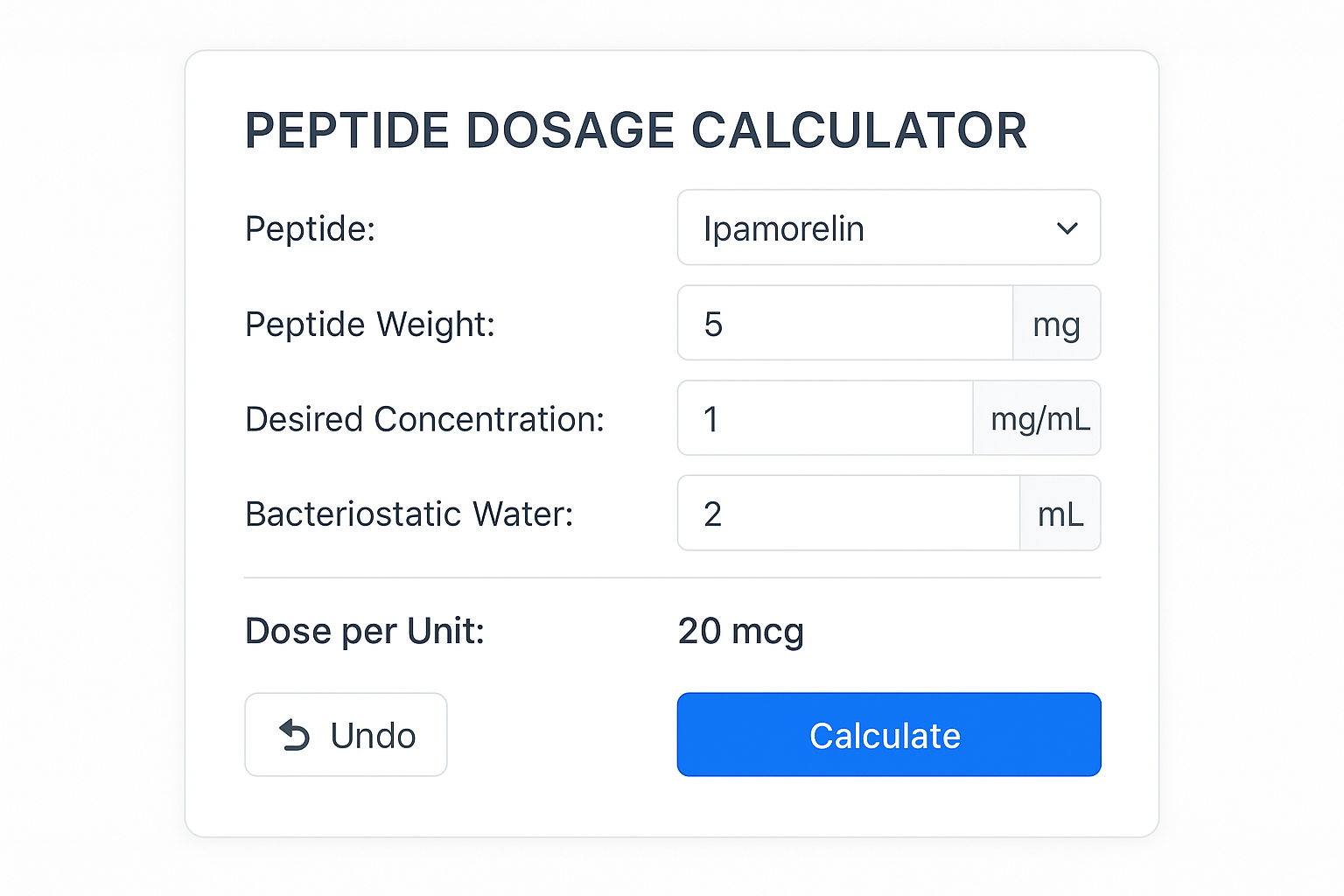
Interactive Element Spotlight: To assist researchers in accurately determining the required volume for their specific peptide and desired dose, an interactive calculator can be incredibly helpful. This tool would allow inputs for peptide vial size, desired dose, and reconstitution volume to output the exact units or milliliters needed on an insulin syringe.
How to Reconstitute GLP-3 and Other Specialized Peptides
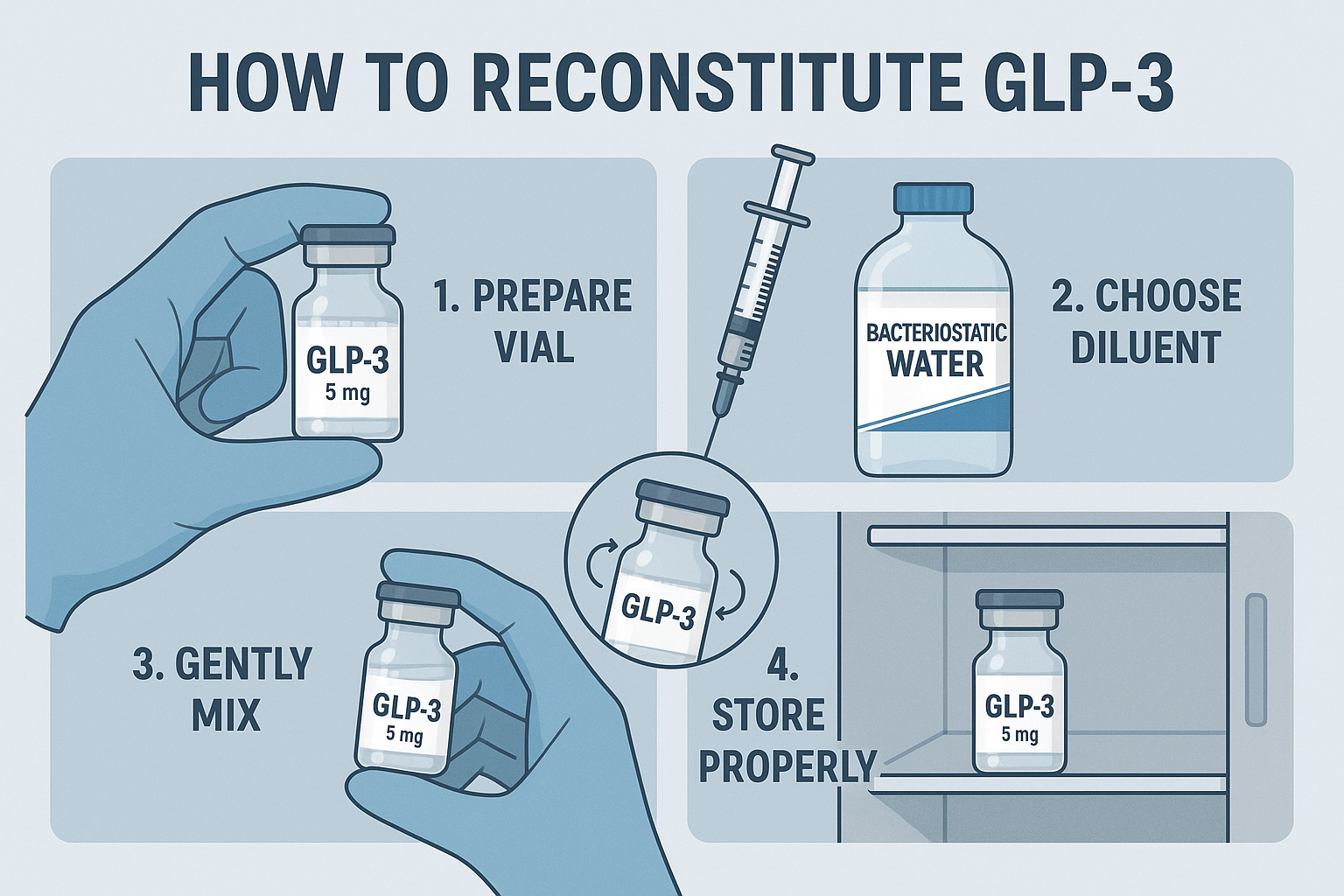
While the general principles of reconstitution apply across most peptides, some, like GLP-3 (Glucagon-Like Peptide-3), might have specific considerations or simply represent another common application of these techniques. Understanding how to reconstitute GLP-3 correctly follows the same meticulous steps outlined earlier, emphasizing gentle handling and sterile practices.
GLP-3 is a less commonly discussed analog in the GLP peptide family compared to GLP-1 agonists, but its reconstitution process is a good example of how to handle any novel or less common peptide.
General Steps for GLP-3 (and similar peptides)
- Verify Peptide Vial Size: GLP-3, like many others, will come in a specific milligram (mg) amount (e.g., 2mg, 5mg).
- Select Bacteriostatic Water: Always use sterile bacteriostatic water for reconstitution to ensure the longest possible shelf life for your reconstituted solution.
- Determine Desired Concentration:
- If you have a 2mg vial (2000mcg) and want a convenient concentration where, say, 10 units on an insulin syringe (U-100) equals 100mcg:
- 100mcg / 0.1ml = 1000mcg/ml
- To get 2000mcg at 1000mcg/ml, you would need 2ml of bacteriostatic water.
- If you have a 2mg vial (2000mcg) and want a convenient concentration where, say, 10 units on an insulin syringe (U-100) equals 100mcg:
- Aseptic Preparation:
- Clean the rubber stoppers of both the GLP-3 vial and the bacteriostatic water vial with alcohol wipes.
- Wear gloves to maintain sterility.
- Slow and Gentle Injection:
- Draw 2ml of bacteriostatic water into a sterile insulin syringe.
- Slowly inject the water into the GLP-3 vial, allowing it to run down the side of the glass. Avoid direct forceful injection onto the peptide powder.
- Gentle Swirling, No Shaking:
- Once the water is in, gently swirl or roll the vial until the GLP-3 powder is completely dissolved. This may take a few minutes. Patience is key.
- Refrigerated Storage:
- Store the reconstituted GLP-3 solution in the refrigerator (2-8°C / 36-46°F) and protect it from light.
- Its stability after reconstitution will likely be a few weeks, but always refer to specific product information if available.
The principles for how to reconstitute GLP-3 are fundamentally the same as for Ipamorelin, tesa, or CJC-1295. The key is consistent application of sterile technique and gentle handling to preserve the peptide’s integrity.
Considerations for Peptides Beyond Standard Subcutaneous Injection
While subcutaneous injection with an insulin syringe is the most common route for many research peptides, some are studied via other methods, such as nasal sprays or oral capsules.
- Nasal Sprays: Peptides like BPC-157 are sometimes explored in nasal spray formulations for systemic or localized effects in the nasal passages or brain. These typically involve reconstituting the peptide in a small volume of sterile saline (not bacteriostatic water, due to benzyl alcohol irritation) and then transferring it to a nasal spray bottle. Dosages are often higher due to lower bioavailability through this route. For example, some researchers explore BPC-157 nasal spray and capsules evidence.
- Oral Capsules: Certain peptides, particularly those with high oral bioavailability or designed to resist gut degradation, may be formulated into capsules. BPC-157 is one such example. Oral dosages are typically much higher than injectable forms due to first-pass metabolism. The “reconstitution” for these is simply consuming the capsule as provided.
- Topical Applications: Peptides like GHK-Cu are well-known for topical applications in skin research. Here, the peptide is often mixed into a cream or serum base. The “dosage” here refers to the concentration within the topical formulation (e.g., 1-3% GHK-Cu) and the amount of cream applied. Discover more about topical GHK-Cu applications.
Regardless of the administration route, careful measurement and preparation are always paramount to ensure the consistency and reliability of research outcomes.
Advanced Considerations for Peptide Dosages and Administration in 2025
As peptide research evolves, so do the nuances of administration and dosing strategies. Researchers in 2025 are increasingly exploring more sophisticated protocols, including peptide stacking, cycling, and precise timing.
Peptide Stacking and Cycling
“Stacking” refers to the concurrent administration of multiple peptides to achieve synergistic effects or target different pathways simultaneously. “Cycling” involves alternating periods of peptide administration with periods of cessation. Both strategies are employed to optimize research outcomes and potentially mitigate receptor desensitization.
- Example: GHRP/GHRH Stack: Combining a GHRP (like Ipamorelin) with a GHRH (like CJC-1295 without DAC) is a classic example of stacking. The GHRP provides a strong pulse of GH release, while the GHRH amplifies this pulse and ensures a more sustained, physiological release pattern. The dosages for each peptide would remain within their typical ranges, but their combined effect is often greater than either alone. For example, a common research protocol might involve 100mcg Ipamorelin + 100mcg CJC-1295 (No DAC) 1-3 times daily.
- Example: Healing Stack: BPC-157 and TB-500 are frequently stacked due to their complementary roles in tissue repair and regeneration. A typical research stack might involve 250mcg BPC-157 daily alongside 2-5mg TB-500 weekly, especially in studies focused on injury recovery. Further research into BPC-157 TB-500 combination research is ongoing.
- Cycling for Effectiveness: Some peptides are cycled to prevent receptor downregulation or to mimic natural biological rhythms. For instance, a growth hormone-releasing peptide might be administered for 8-12 weeks, followed by a 4-week break, to maintain sensitivity.
Timing of Administration
The timing of peptide administration can significantly influence their effects, particularly for those that interact with hormonal rhythms.
- Before Bed: Many GHRPs and GHRH analogs (like Ipamorelin, tesa, and CJC-1295) are often administered before bedtime. This timing aims to coincide with the body’s natural pulsatile release of growth hormone during sleep, potentially enhancing its effects.
- Fasting State: Administration on an empty stomach (e.g., 30-60 minutes before a meal or several hours after) is often recommended for GH-releasing peptides. This is because food, especially carbohydrates and fats, can blunt the growth hormone response.
- Post-Workout: Peptides involved in repair and recovery, such as BPC-157, might be administered post-workout to support muscle and tissue healing during the critical recovery window.
Dilution and Accuracy for Micro-dosing
For very small doses, especially when using highly potent peptides, accurate dilution is paramount. If a standard reconstitution leads to a concentration that is too high for precise drawing on an insulin syringe, further dilution might be necessary.
- Example: If 10 units = 100mcg, and your desired dose is 10mcg, drawing 1 unit precisely can be challenging on a U-100 syringe. In such cases, you might further dilute your reconstituted solution.
- If you have a 1ml solution containing 1000mcg (1mg/ml), drawing 0.1ml of this solution and mixing it with another 0.9ml of bacteriostatic water would create a 1ml solution containing 100mcg. Now, 10 units of this new solution would be 10mcg, making precise measurement easier.
- This secondary dilution requires even more meticulous sterile technique and careful labeling to avoid confusion.
Understanding Syringe Markings and Conversions
Most researchers use U-100 insulin syringes, which are designed for injecting small, precise volumes.
- A U-100 syringe holds 1ml (or 1cc) of liquid.
- It is marked from 0 to 100 units.
- Therefore, 10 units = 0.1ml, 50 units = 0.5ml, and 100 units = 1ml.
Understanding this conversion is fundamental to accurately drawing the correct dose after reconstitution. If your reconstitution results in 100mcg per 0.1ml (10 units), then knowing your desired dosage directly translates to a specific number of units on the syringe.
Table: Insulin Syringe Unit-to-Volume Conversion
| Syringe Units | Volume (ml) |
|---|---|
| 1 unit | 0.01 ml |
| 5 units | 0.05 ml |
| 10 units | 0.1 ml |
| 20 units | 0.2 ml |
| 50 units | 0.5 ml |
| 100 units | 1.0 ml |
This table is a handy reference for quickly converting calculated peptide dosages into the corresponding syringe volume.
Pull Quote: “The research landscape for peptides in 2025 demands not just knowledge of individual peptide dosages, but also a sophisticated understanding of how they interact in stacks, how timing optimizes their effects, and the absolute precision required for micro-dosing.”
Quality and Sourcing of Research Peptides
The efficacy and safety of any peptide research ultimately depend on the quality and purity of the peptides themselves. In 2025, researchers are more vigilant than ever about sourcing their compounds from reputable suppliers.
- Purity Standards: High-quality research peptides should come with a Certificate of Analysis (CoA) from a third-party lab, verifying their purity (typically >98-99%) and molecular structure. Impurities can significantly affect research outcomes.
- Third-Party Testing: Suppliers that provide readily accessible third-party testing results demonstrate transparency and commitment to quality. This helps ensure that what’s on the label is actually in the vial.
- Reputable Suppliers: Choosing a supplier with a strong track record, positive researcher feedback, and transparent practices is crucial. Websites like Pure Tested Peptides offer a range of peptides specifically for research purposes.
- Proper Storage and Shipping: The supplier should ensure that peptides are stored and shipped under appropriate conditions (e.g., cold chain for lyophilized peptides) to maintain their stability before they reach the research lab.
Researchers seeking to build a robust peptide library for their studies should prioritize suppliers that adhere to these stringent quality controls. For more information on ensuring the quality of your research materials, consult resources on building a diverse peptide library with Pure Tested Peptides.
Conclusion
Understanding dosages for peptides, from the initial reconstitution of compounds like dosage Ipamorelin, dosage tesa, and dosage CJC-1295, to the practical intricacies of how to reconstitute GLP-3, forms the bedrock of credible and impactful peptide research. In 2025, the scientific community continues to push the boundaries of knowledge surrounding these remarkable molecules. Precision in preparation, accurate measurement with insulin syringes, appropriate storage, and adherence to established research protocols are not merely suggestions but absolute requirements.
By mastering the techniques of reconstitution, carefully calculating diluent volumes, understanding syringe unit conversions, and adhering to typical dosage ranges, researchers can maximize the integrity and reliability of their studies. The dynamic nature of peptide research also calls for an awareness of advanced strategies like stacking, cycling, and optimal timing, allowing for more nuanced and effective experimental designs. As we move forward, the commitment to high-quality peptides from reputable sources remains paramount, ensuring that scientific discoveries are built upon a foundation of purity and efficacy.
Actionable Next Steps for Researchers:
- Always Double-Check Calculations: Before reconstituting, meticulously calculate the bacteriostatic water volume needed to achieve your desired concentration.
- Practice Aseptic Technique: Ensure a sterile environment when handling peptides to prevent contamination and maintain product integrity.
- Invest in Quality Syringes: Use high-quality U-100 insulin syringes for accurate and consistent dosing.
- Reference Specific Product Information: While this guide provides general ranges, always consult the specific product information or Certificate of Analysis for precise handling and storage recommendations for each peptide.
- Stay Informed: Continuously review current scientific literature and research protocols for updates on peptide administration and dosing SEO Meta Title: Peptide Dosages 2025: Ipamorelin, tesa, CJC-1295, GLP-3
SEO Meta Description: Explore typical research dosages for peptides like Ipamorelin, tesa, and CJC-1295 in 2025. Learn reconstitution, syringe volumes, and how to reconstitute GLP-3.
strategies.
Peptide Dosage & Reconstitution Calculator
Use this tool to determine reconstitution volumes and syringe units for accurate peptide dosing. This tool is for research purposes only.
Calculation Results:
Concentration: 0 mcg/ml
Volume per Desired Dose: 0 ml
Units on U-100 Syringe: 0 units
Total Doses per Vial: 0 doses
Note: Always use sterile bacteriostatic water for reconstitution. This calculator provides estimated values; precise measurement tools and aseptic technique are crucial.

Leave a Reply
Want to join the discussion?Feel free to contribute!